|
Ashwood FertilityCare Center is honored to Feature NaPro Technology through 4 amazing Medical Consultants!
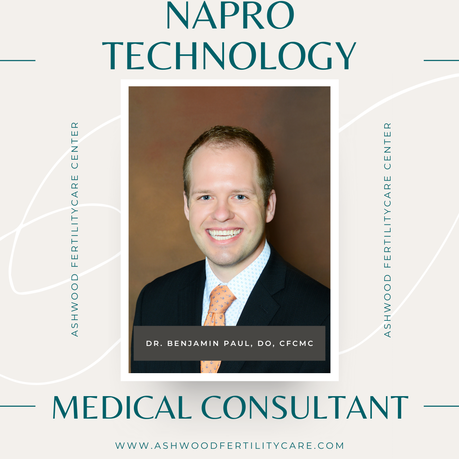
We would like to introduce you to each one of them. Please share your stories of how these amazing Medical Providers have cared for you with NaPro Technology and Restorative Reproductive Technologies which work cooperatively with the woman's natural cycles using the woman's Creighton Model FertilityCare chart. Dr. Benjamin Paul, DO, CFCMC joined the Ashwood FertilityCare Team this year after completing his residency at University of Minnesota-Mankato. In September Dr. Paul completed his NaPro Technology training at the Saint Paul VI Institute for Human Reproduction. Dr. Paul and his wife, Ashley (who also serves as a FertilityCare Practitioner) have made Humboldt, IA their home and they are excited to serve the women/couples of Humboldt county and beyond! The Pauls have 2 beautiful daughters and they serve as a family. Dr. Paul says: "I chose family medicine because it is a specialty that focuses on the individual person and I cherish the relationships I have with my patients. I provide courteous holistic care where I am loyal to my patients." "I felt called by God to be a physician and have been given the opportunities and skills to follow that calling. My passion is to assist others to find health, so they can pursue their own passions." The first step to receiving a referral to a NaPro Medical Consultant is to begin charting with the Creighton Model FertilityCare System. Ashwood FertilityCare Center offers free monthly Introductory Sessions to begin the journey of learning the charting process to be used in the testing, diagnosis and cooperative treatment of most underlying menstrual cycle issues including PMS, unknown infertility, PCOS and Endometriosis. Join us at our next Intro Session Webinar to learn more! www.ashwoodfertilitycare.com/get-started
0 Comments
Life is full of miracles that change our world forever! Our little son Simon was nothing short of that miracle to our family! Our story of pregnancy began as anyone would expect. Having been newly married in June of 2016, being open to life and finding out our family was growing by one in the fall of 2016 and anxiously dreaming and anticipating our growing family was an exciting and unknown chapter that we had never yet entered.
Our pregnancy seemed nothing short of ordinary until I began noticing having increased swelling of my lower legs and slightly increased puffiness to my face. Assuming this was just a typical response to the later stages of pregnancy, I took steps of wearing compression socks and elevating my legs to help with increased inflammation. Not long after however, my symptoms began to worsen. One morning I woke up with a splitting headache and just feeling "off". My husband took my blood pressure and we soon realized that my pressures were highly elevated. I called my OB for triage and fortunately was able to be seen that afternoon for an urgent OB clinic visit; labs were ordered, urine analysis undergone, and an ultrasound was performed to check on our son. It was then that our OB doctor walked in and shared the news that our son was not receiving the proper blood flow to grow properly, there was excess protein in my urine, abnormal blood levels, and that our next step would be to transfer emergently to a larger city with a NICU available as both our son and I would need added support with a critical timeline. So many thoughts were racing through my head. Would our son be healthy enough to survive delivery? How would I be able to deliver our son when we hadn’t even had a chance to attend any birthing classes yet? What were those first moments as a family going look like at his birth? These questions along with so many others came over me. We made the decision to rush by our own vehicle to St. Louis (a 2-hour drive from where we were currently living at the time) to be admitted to the hospital on bedrest and close observation. Over a 24-hour period, our pregnancy went from uneventful to life altering when our son was just 26 and 5 days old gestationally. I couldn’t help but wonder, how could this be happening to our family and why was my body not able to do what I always imagined pregnancy and giving birth to look like? I was given the diagnosis of severe pre-eclampsia which progressed quickly into HELLP syndrome and subsequently caused our son to have fetal growth restriction of weight below the 10th percentile for his age called IUGR. Our prognosis was poor and the plan to begin corticosteroid injections to stimulate our son's lungs, medications to manage blood pressure, constant fetal monitoring, and complete bedrest was begun. Delivery was anticipated to be anywhere from immediately to 3 months from admission to await our son arriving as close to term as possible. Our hearts were yearning for his delivery to be as close to term delivery as possible, but the medical signs remained to show us otherwise. |
Author
Archives
September 2021
Categories
All
|


 RSS Feed
RSS Feed